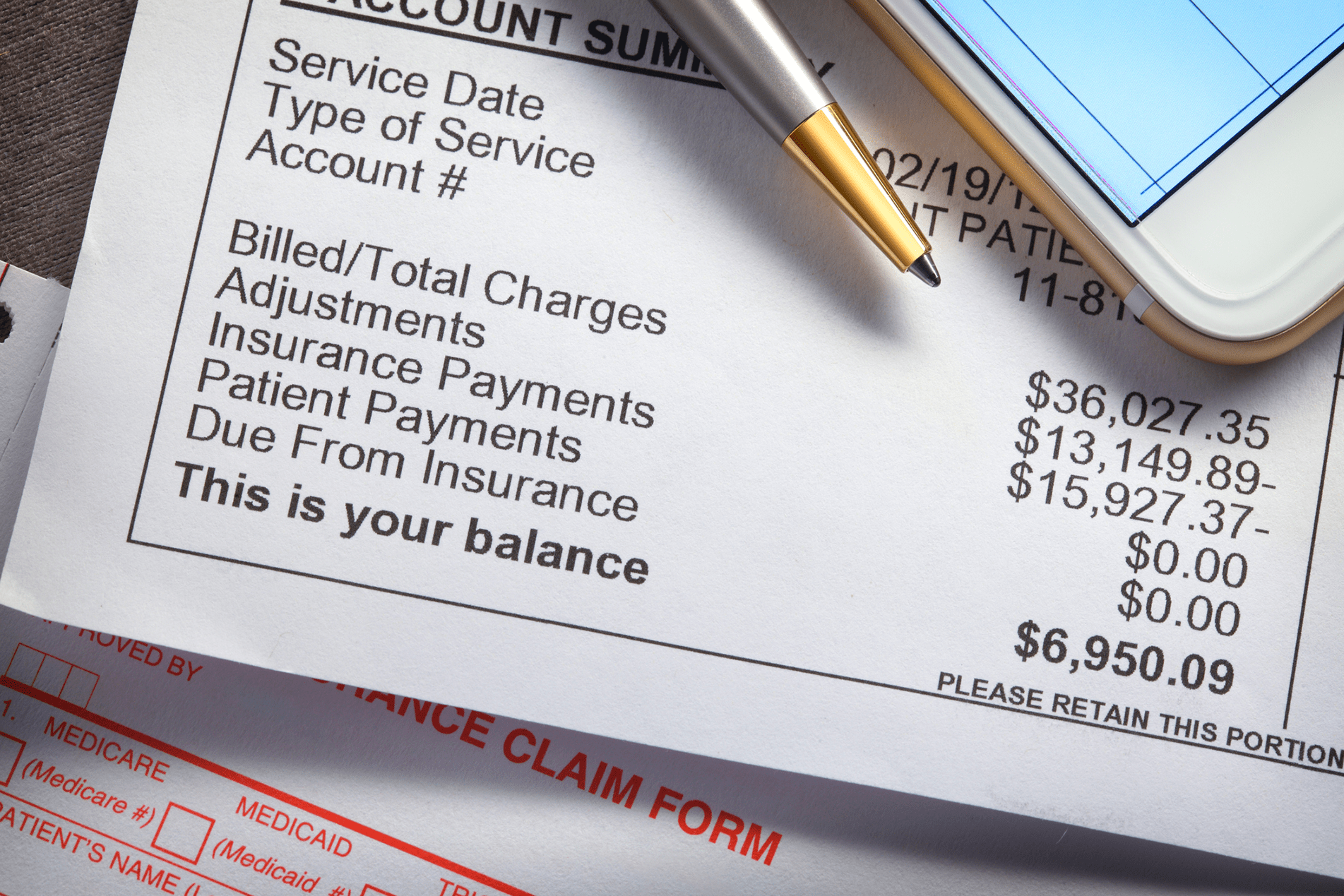
Artificial Intelligence (AI) is one of the most talked-about technologies in healthcare today, especially in the realm of Revenue Cycle Management (RCM). Promises of increased efficiency, reduced administrative burden, faster reimbursements, and higher collection rates have made AI a hot topic. But is it all hype, or is there real value for medical practices looking to improve their financial performance and patient experience?
As healthcare providers face growing pressure to do more with less, understanding the true impact of AI on revenue cycle operations is critical. Many organizations are evaluating whether AI can offer practical improvements or if it’s just the latest tech buzzword. In this article, we’ll cut through the noise to examine what AI can and can’t do, explore real-world applications, and outline how solutions like Rivia Health harness AI to make a measurable difference in patient payment outcomes.
What is AI in Revenue Cycle Management?
AI in RCM refers to the use of machine learning algorithms, natural language processing (NLP), robotic process automation (RPA), and advanced analytics to improve how healthcare providers manage the financial aspects of patient care. This includes everything from eligibility verification and claims processing to patient billing, communication, and collections.
Unlike traditional automation, which follows static, pre-programmed rules, AI systems can learn from data patterns, make predictive decisions, and adapt over time. This allows for more intelligent workflows, improved accuracy, and personalization that’s unattainable through manual or rule-based systems alone.
Common AI-driven capabilities in RCM include:
- Predicting which accounts are most likely to be paid
- Automating prior authorizations and eligibility checks
- Extracting relevant data from unstructured documents (e.g., EOBs, clinical notes)
- Identifying coding and billing errors before claims are submitted
- Customizing patient payment reminders based on communication preferences and behavior
The Hype: What AI Promises
- 100% Automation
Vendors often claim AI can fully automate your entire revenue cycle, eliminating the need for human involvement. While AI can streamline many tasks, it’s far from replacing the nuanced judgment, empathy, and communication skills that healthcare staff provide. Clinical and financial decisions still require human oversight.
- Plug-and-Play Simplicity
Another myth is that AI solutions are instantly deployable and require minimal effort to integrate. In reality, AI tools are only as effective as the data they access and the infrastructure they’re built upon. Poor data quality, siloed systems, and lack of interoperability can significantly hinder AI’s potential.
- Immediate ROI
AI is often marketed as a fast-track to financial improvement. While AI can drive meaningful efficiencies, expecting instant returns sets unrealistic expectations. Effective AI implementation involves data training, testing, iteration, and ongoing monitoring to achieve sustained performance gains.
- Replacing Your Team
Contrary to fear-based narratives, AI is not about eliminating jobs. The best solutions use AI to automate repetitive, low-value tasks so staff can focus on high-value activities like patient engagement, strategic planning, and problem-solving.
- One-Size-Fits-All Solutions
AI platforms vary widely in quality, functionality, and relevance. A generic tool not tailored for healthcare or your specific practice size, specialty, or workflow may fall short. Customization and domain expertise are essential for AI to succeed in RCM.
The Reality: Where AI Delivers Real Value
Despite the inflated promises, AI can offer substantial advantages when implemented strategically. Here are six key areas where AI is already transforming revenue cycle management:
- Enhanced Patient Outreach and Communication
AI can tailor communication strategies based on patient behavior, demographics, past interactions, and payment history. For example, platforms like Rivia Health use AI to optimize the timing and channel (text vs. email) of reminders, increasing the likelihood of patient engagement. Personalization leads to better response rates and ultimately faster payments.
- Intelligent Claims Scrubbing and Denial Prevention
AI algorithms can analyze claims pre-submission to identify common coding errors, documentation mismatches, and missing fields that could trigger denials. By proactively catching these issues, practices can improve their clean claim rate, shorten reimbursement cycles, and reduce costly rework.
- Predictive Analytics for Collections
Not all unpaid balances are equal. AI can categorize accounts by their likelihood to pay, allowing billing teams to prioritize efforts and allocate resources more efficiently. This risk stratification approach improves recovery rates and minimizes time spent on uncollectible balances.
- Automating Routine, Time-Consuming Tasks
Tasks such as eligibility verification, insurance authorization, and data extraction from scanned documents are time-consuming and error-prone when done manually. AI-powered bots can handle these processes quickly and accurately, reducing administrative overhead and increasing productivity.
- Real-Time Performance Dashboards and Insights
AI-driven analytics platforms provide real-time visibility into revenue cycle metrics, such as patient payment trends, denial rates, and team productivity. With actionable insights at their fingertips, revenue cycle leaders can make data-informed decisions and intervene proactively when issues arise.
- Improved Patient Engagement and Experience
AI enables more empathetic and humanized communication at scale. From offering smart payment plan options to sending reminders in simple language, AI improves the billing experience for patients—leading to greater satisfaction and on-time payments.
AI and the Patient Experience
The patient experience is increasingly recognized as a critical component of the revenue cycle. When patients receive clear, timely communication and flexible payment options, they are far more likely to fulfill their financial responsibilities.
AI plays a vital role in making this possible by:
- Analyzing patient payment behavior to determine the best outreach strategy
- Sending reminders at optimal times to increase action rates
- Offering payment plans that reflect the patient’s historical preferences or financial circumstances
- Using natural language generation to create messages that are understandable, friendly, and actionable
The result? A more empowered patient who feels respected and in control of their financial journey.
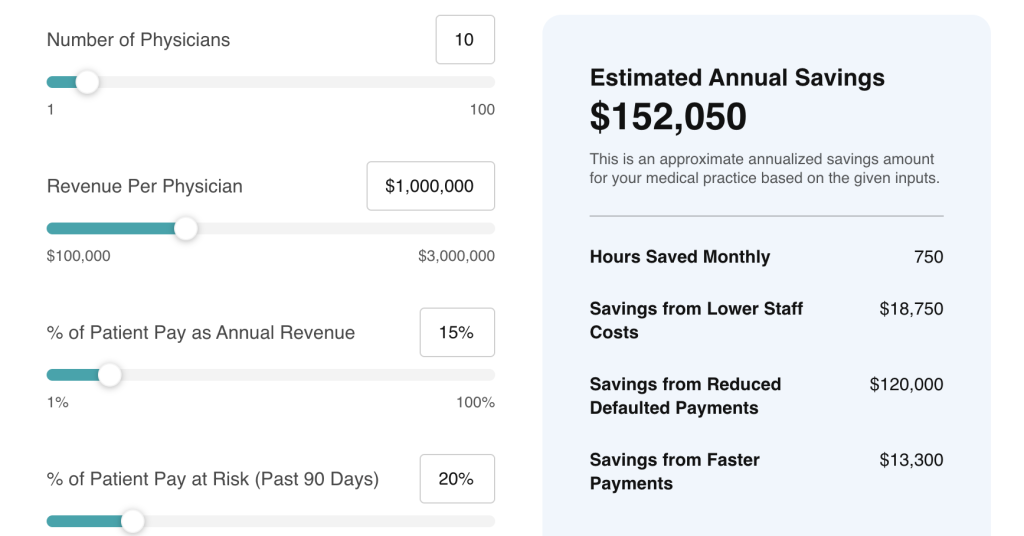
How Rivia Health Uses AI to Improve Patient Collections
At Rivia Health, we believe AI should serve a purpose: to make billing and collections simpler, smarter, and more patient-friendly. Our platform leverages AI to:
- Automate personalized patient outreach through secure, HIPAA-compliant text and email
- Optimize communication timing and format for maximum engagement
- Deliver a frictionless, login-free payment experience on mobile devices
- Support payment plans and multiple payment methods
- Reduce manual work for staff with automated follow-up tasks and performance tracking
We integrate directly with leading EHR and billing systems like athenahealth to provide a seamless and intelligent billing experience. This not only improves collection rates but also enhances the overall patient experience—turning what was once a pain point into a competitive advantage.
Final Thoughts: Embrace AI, But Stay Grounded
AI in revenue cycle management is not a silver bullet—but it is a game-changing tool when used correctly. To harness its full potential, healthcare practices must separate realistic, results-driven capabilities from the hype. Implementing AI with a clear strategy, high-quality data, and the right partner is the foundation for success.
By leveraging AI to streamline workflows, personalize patient communication, and reduce administrative burden, practices can drive better financial outcomes while freeing staff to focus on patient care.
Ready to explore how AI-powered billing from Rivia Health can help your practice collect more, faster, and with less effort? Let’s talk.