The healthcare industry has experienced a profound transformation in recent years, particularly in how providers are reimbursed for services. One of the most significant developments is the increasing financial responsibility now placed on patients. With the rise of high-deductible health plans, increased co-payments, and out-of-pocket maximums, patient payments now constitute a much larger portion of healthcare revenue. This shift has placed new pressure on medical practices and health systems to rethink and revamp their billing and collection strategies in order to stay financially healthy and meet patient expectations.
Patient pay is not a passing trend—it’s the new norm. The challenge facing providers? Many still struggle to collect what they’re owed—and to do it efficiently. Fortunately, the right combination of technology and strategy can dramatically improve collection efforts. Digital tools can simplify the payment process, enhance the patient experience, reduce the administrative burden, and ultimately boost revenue. Providers that embrace these innovations can turn patient pay from a pain point into a performance driver.
In this article, we’ll dive into why patient payments are more critical than ever, highlight the common roadblocks to effective collections, and present actionable strategies to collect more, faster. We’ll also explore how digital engagement solutions like those offered by Rivia Health can help modern practices thrive in today’s payment landscape.
Why Patient Pay Matters More Than Ever
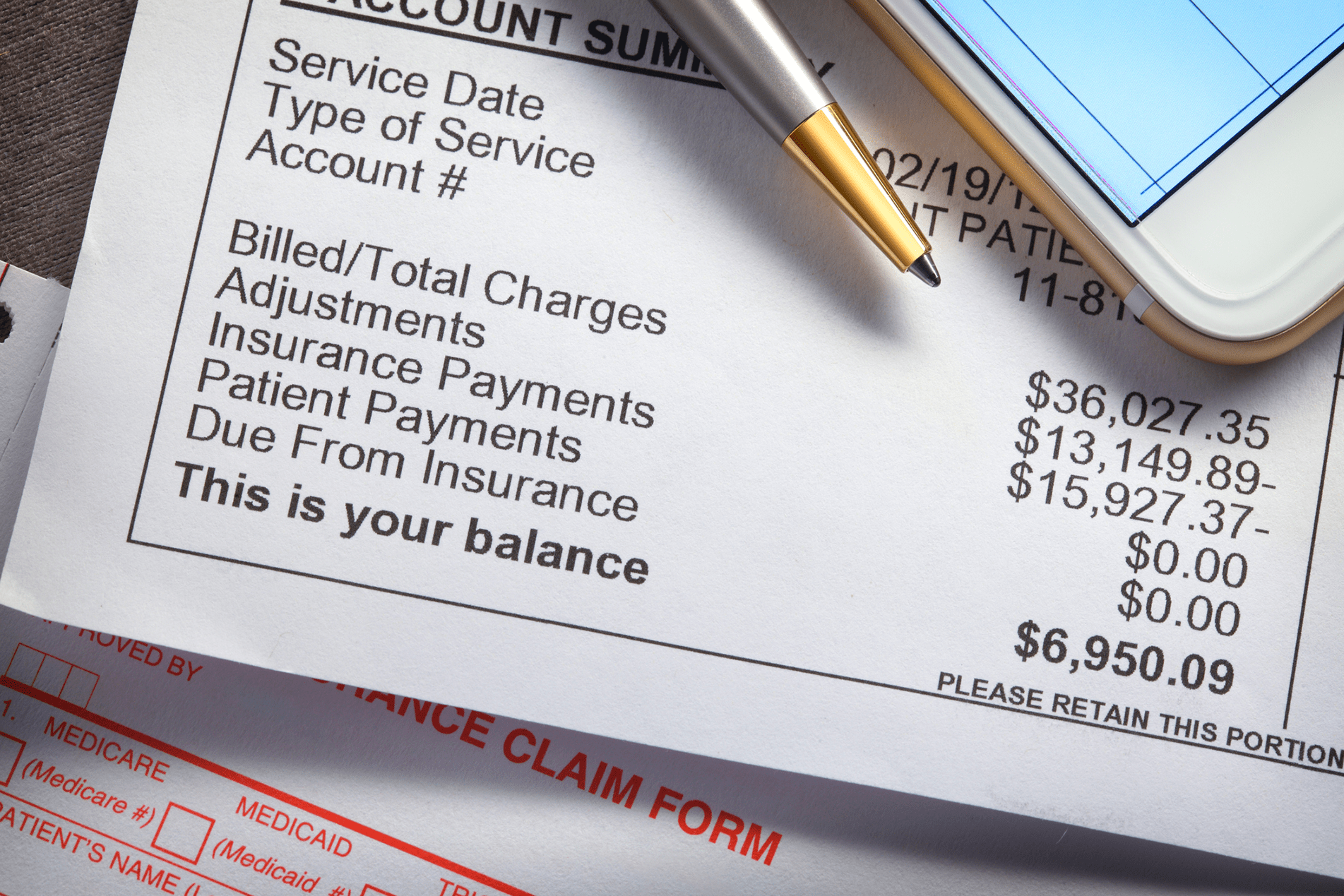
As the healthcare payment landscape evolves, the share of financial responsibility falling on patients continues to grow. According to industry data, patient payments now represent nearly 35% of total provider revenue—a figure that is expected to increase in the coming years. Despite this growth, many providers still rely on outdated billing systems that were not designed for today’s consumer-driven payment environment. Manual processes, long delays in billing, and reliance on paper statements contribute to lost revenue and patient dissatisfaction.
On average, only about 20% of patient balances are collected after a visit, leading to massive gaps in cash flow. Worse, the longer a bill remains unpaid, the lower the chances of ever collecting it. This is a major revenue drain that many practices simply can’t afford to ignore. The key to closing this gap is to engage patients with tools that match their communication preferences—primarily mobile—and empower them to take swift action.
A mobile-first, user-friendly, and personalized payment experience isn’t just a convenience—it’s a competitive necessity. Patients have become consumers who expect the same ease of use they get from retail, banking, and other industries. Practices that adapt to these expectations will enjoy better patient satisfaction and healthier bottom lines.
Common Barriers to Patient Payment Collection
Before improving patient collections, it’s essential to understand what’s preventing timely payment. Several recurring issues plague medical practices, all of which can be addressed with the right technology:
- Lack of clarity: Confusing bills with complex jargon leave patients unsure of what they owe, why they owe it, and how to resolve it.
- Cumbersome processes: Systems that require logging into a portal, remembering a password, or mailing a physical check create significant friction.
- Limited payment flexibility: Many practices don’t offer modern payment methods or installment plans, deterring patients from completing transactions.
- Delayed billing: Sending a bill weeks or even months after a visit reduces urgency and increases the risk of non-payment.
- Staff constraints: Administrative teams are often overburdened, spending hours each week on manual follow-ups, reducing their capacity for high-value work.
These issues are all solvable with technology designed specifically for healthcare revenue collection.
Strategies for Faster, More Effective Patient Collections
To increase collections and reduce administrative burden, practices must adopt a streamlined, patient-friendly billing experience. Here are five actionable strategies:
1. Go Mobile-First
Patients live on their phones. Text messages and emails are opened and acted on much more quickly than traditional mail. Practices should implement mobile-first solutions that allow patients to pay through a secure, personalized link—no login required. This removes barriers and dramatically shortens the payment timeline.
Bonus tip: Send reminders around the times patients are most likely to act, such as early evening or after typical work hours, and consider syncing reminders with payday cycles for better timing.
2. Offer Multiple Payment Options
One-size-fits-all doesn’t work for payments. Some patients want to pay in full using credit or debit cards; others prefer Apple Pay, Google Pay, or even ACH. Some need a payment plan to break a large bill into manageable installments. Giving patients options—without needing to call the office—increases the likelihood they’ll pay promptly.
Bonus tip: Consider offering autopay for recurring care needs to reduce missed payments and ease the burden on chronic care patients.
3. Be Transparent and Timely
Transparency is key to trust. Patients want to know what they’re paying for and when they need to pay it. Bills should be clear, itemized, and delivered shortly after the appointment to maintain context. The more transparent and immediate the billing, the more confident patients feel about making a payment.
Bonus tip: Add explanations of benefits or cost breakdowns directly within digital statements and offer quick support via chatbot or a live representative.
4. Automate Follow-Ups
Manual reminders take time and often fall through the cracks. Automating follow-ups ensures consistent communication while saving staff hours each week. Reminders can be sent via text or email on a set schedule, triggered by payment status or patient behavior. Personalization—like including the patient’s name and provider—helps increase engagement.
Bonus tip: Vary your outreach cadence and channel (text/email) to optimize engagement based on patient preferences and responsiveness.
5. Empower Staff with Smart Tools
Technology isn’t just for patients—it’s for staff, too. Giving front office and billing teams access to intuitive dashboards, balance alerts, and conversation templates helps them address payment issues efficiently and confidently. Training staff to have empathetic, clear payment conversations also increases success rates.
Bonus tip: Implement gamification or performance tracking to incentivize effective collection efforts among your team.
How Rivia Health Helps You Collect More, Faster
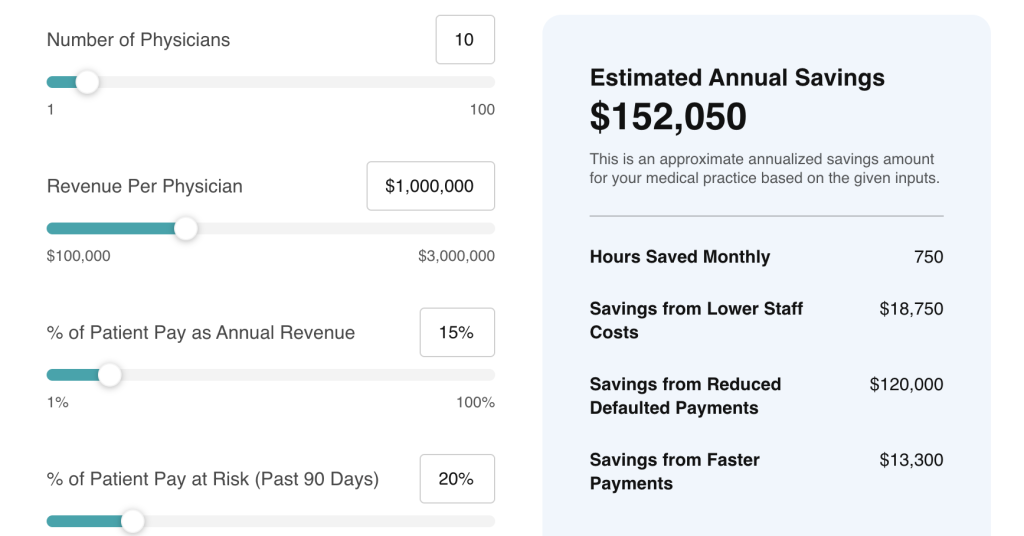
Rivia Health is built for the modern healthcare economy. Our platform simplifies patient payments through automation, personalization, and seamless integration with popular EHR and billing systems like athenahealth. With our solution, you can:
- Send personalized, login-free payment reminders via text and email
- Enable payment directly from any device—no accounts or passwords needed
- Offer flexible payment options, including digital wallets and payment plans
- Reduce the burden on staff with automated outreach and follow-ups
- Gain real-time insights into collections and patient responsiveness
With Rivia Health, practices achieve faster payment cycles, higher collection rates, and happier patients—all while freeing up internal resources for more strategic work. Our approach enhances both the financial health of your practice and the satisfaction of the people you serve.
Final Thoughts: Make Patient Pay a Strategic Advantage
There’s no denying it: patient pay is here to stay—and its influence is only growing. Practices that cling to outdated billing methods will continue to face increasing collection challenges, missed revenue opportunities, and rising administrative costs. In contrast, those that adopt smarter, more patient-friendly strategies will be well-positioned to succeed.
By investing in mobile-first communication, payment flexibility, and workflow automation, your practice can reduce friction in the billing process and improve financial outcomes. The result? A win-win for both your team and your patients.
At Rivia Health, we specialize in helping healthcare organizations modernize the patient payment experience. Whether you’re looking to decrease no-shows, increase collections, or simply reduce manual tasks, our platform is purpose-built to drive results.
Let’s connect and build a smarter approach to patient payments—together.