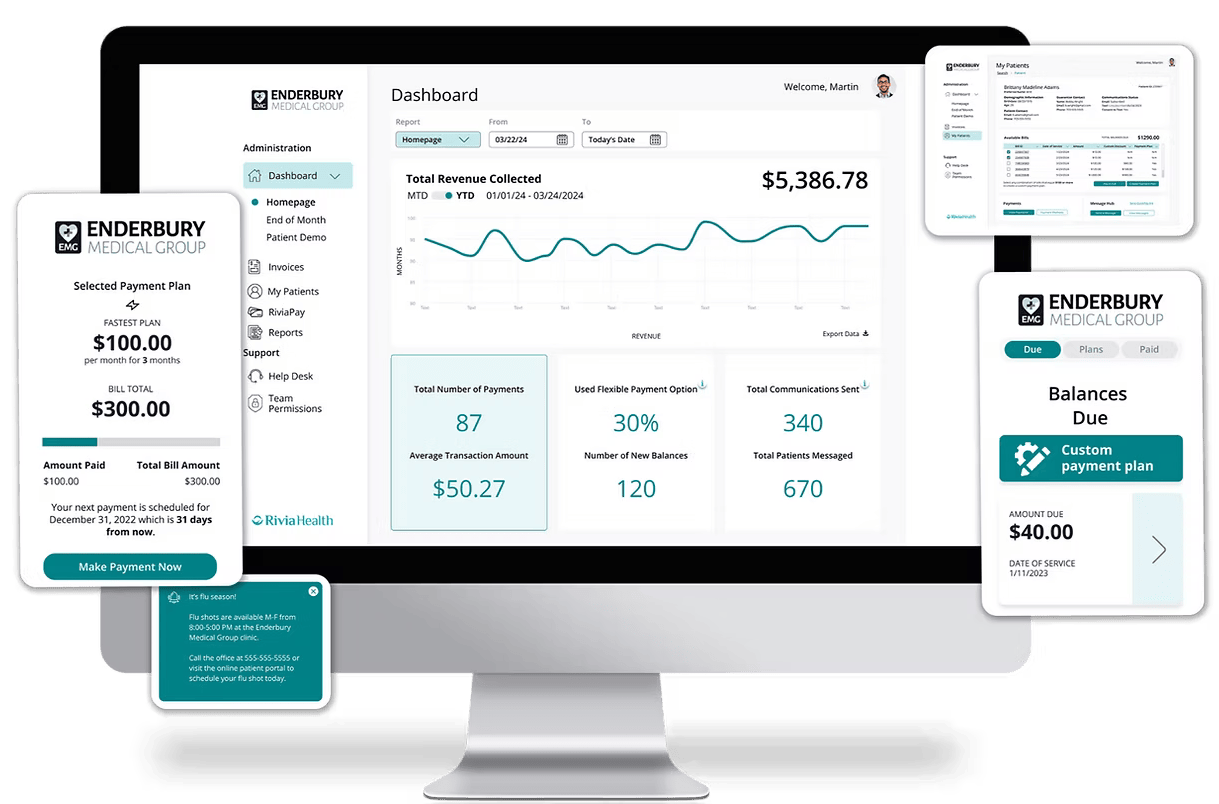

RiviaConnect elevates your financial management with real-time data and customizable tools. Easily manage patient AR, set optimal payment terms, and empower your staff to implement them effectively. Leverage patient demographics to craft targeted communication strategies, ultimately boosting your revenue cycle, reducing bad debt, and enhancing the patient financial experience.
Track revenue instantly with a real-time financial dashboard, providing visibility into total revenue and patient plan utilization
Streamline front desk operations with a comprehensive patient hub, simplifying patient information management
Gain valuable patient demographics insights, including at-a-glance tracking of communication metrics and consent rates
Our robust payment platform comes with flexible communication options, matching the needs of your practice.
Based on patient engagement, stage in payment lifecycle, and by bill type
Campaigns tailored for each practice type, ensuring the highest patient engagement
Messages sent ahead of appointments, reducing expensive no-shows
Pre-service balances and copays through post-service balances and late payments







Time saved from crafting and sending batched patient messages manually, fielding inbound calls regarding payments, placing outbound calls regarding payments, collecting payments over the phone, and setting up payment plans.
Learn why Rivia Health is a leader in healthcare revenue cycle management.

Rivia Health offers customized patient communication campaigns for patient appointments, copay collection, patient statements, and outstanding accounts receivable (AR). Campaigns are optimized to maximize patient engagement to capture the patient into the payment experience, reducing the need for manual intervention and follow up.
Tailored toward the highest user engagement [text, email]
Designed specifically for outstanding patient accounts receivable
Provides patients with confidence in a secure payment process

Rivia Health’s participation in the athenahealth Marketplace enables turn-key integration with existing athenahealth solutions. Seamless, bi-directional integration allows copays and patient balances to be automatically posted directly into athenaCollector®, allowing staff to focus on other tasks. No IT support required and under 5 hours of staff time to go live!
Completed as soon as an Authorization and Consent is completed.
Provides the most up-to-date information on the patient balance. Rivia Health seamlessly posts payments back into athenaCollector®
Payments are processed with Athena’s CCP platform as well as other third-party e-commerce tools

Quick, 1-time payment option or pay over the phone with interactive voice response
Gives patients options to sign up for recurring payment plans to take the guess work out of making payments
-Patients can view their bill details in an easy, user-friendly format
-Patients have the option to schedule a future payments
-Receipts are sent automatically when the payment is processed
–Integrated with Athena CCP and Stripe
Select a percentage or dollar amount that applies to a threshold as a discount and incentive for patients to pay a bill in full
Banners on the payment dashboard call out bills that qualify for a custom discount.


Seamlessly bundle multiple statements into one payment plan, accommodating patients with recurring weekly or monthly appointments. Enjoy default access to bundled payment functionality, automatically included with Rivia Health.
Various bills are added together to create one payment plan as long as a minimum threshold is reached.
All bills listed for a patient can be added to create a custom plan.
Find answers to the most common technical questions about Rivia Health and our robust payment platform.
Yes -- you can determine the minimum balance that qualifies for a payment plan and how long you are willing to give patients to complete the payment plan. Rivia Health will use those two rules to automatically generate options for patients.
Yes, patients can reply STOP to texts or unsubscribe from our emails. This will only remove them from Rivia Health communications so your practice will still be able to reach them via athena communicator for apt reminders and other communications.
Yes, we have completed a 3rd party risk evaluation. Our payment platform follows a 3-step verification process. We operate under a BAA agreement with our customers and do not update patient demographic information in our system. We rely on the demographic information in the customer's system of record.
In order to offer a competitive, flat-model rate, our team will prepare a personalized analysis that looks at three factors:
Rivia Health has a support team that handles "front-line" patient support for your team. Our staff will answer any questions that come through text and email within our capability. If we cannot answer the question, we will forward the conversation history with the patient ID to your team via a secure email.
Yes. We can collect copays if the copay amount is entered into the copay field. We start communicating two weeks prior the appointment and stop accepting payment one hour prior to the appointment to prevent any data confusion as to whether or not the patient has paid at the time of service.
We don’t write card-on-file data back into the EMR system, but we do have it saved in the RiviaPay system to enable patients to keep a card on file and to run payment plans automatically for each payment installment. Patients can also save a card in our system to use at a later date.
Yes, the timing and frequency of our campaigns are customizable to meet your workflows. However, our campaigns are designed to perform optimally based on user behavior data across about 200 customers data analysis and a period of 4 years.
From faster collections to reduced administrative burden, see how our partners are making a measurable impact with Rivia.

Revenue Integrity Manager
“Working with Rivia Health has been an absolute pleasure. Their team of skilled professionals is not only knowledgeable in their field but also dedicated to providing top-notch service and support. I cannot recommend Rivia Health highly enough for any business seeking help with collections. We’ve been working with Rivia for over a year now and have only heard great things from our patients about how easy it is to navigate electronic payment software.”
Suzi Green
“Moving to Rivia Health for our practice payments/collections has been one of the best things we have ever done. Their support team has been great to work with and so very helpful! The implementation was 100% painless, the collection rate is amazing, and I would recommend anyone to work with Rivia Health.”


Chief Financial Officer
“We’ve worked with the Rivia team for 6 months with total satisfaction. They have delivered everything they promised. Zero complaints from our patients using their service. Adding their product to the supplement Athena’s processes (patient statements) has significantly improved our post-visit collections.”

Prior to going live with Rivia Health, Lake City had 51% of patient balances that were greater than 90 days old. With Rivia Health, now only have 16% of patient balances greater than 90 days old!

Director of Revenue Cycle Management
“We started using Rivia Health in January of 2023 and each month we have continued to collect on patient accounts that we otherwise may not have. Rivia Health integrates with our EMR system and pulls the data they need so there is one less project/report on my plate. I’m very pleased with our partnership with Rivia Health and would definitely recommend them.”
See how much your practice could save and collect with Rivia Health. Our quick ROI calculator gives you a personalized estimate in under 60 seconds—no commitment, just insights.